Academic Emergency Medicine
- HINTS and STANDING tests reached high sensitivities at 97% and 94% and NPVs at 99% and 98%, respectively. The ABCD2 score failed to predict half of central vertigo cases and had a sensitivity of 55% and a NPV of 87%. The STANDING test was more specific and had a better positive predictive value (PPV; 75% and 49%, respectively; positive likelihood ratio [LR+] = 3.71, negative likelihood ratio [LR–] = 0.09) than the HINTS test (67% and 44%, respectively; LR+= 2.96, LR– = 0.04).
- Conclusions: In the hands of EPs, HINTS and STANDING tests outperformed ABCD2 in identifying central causes of vertigo.
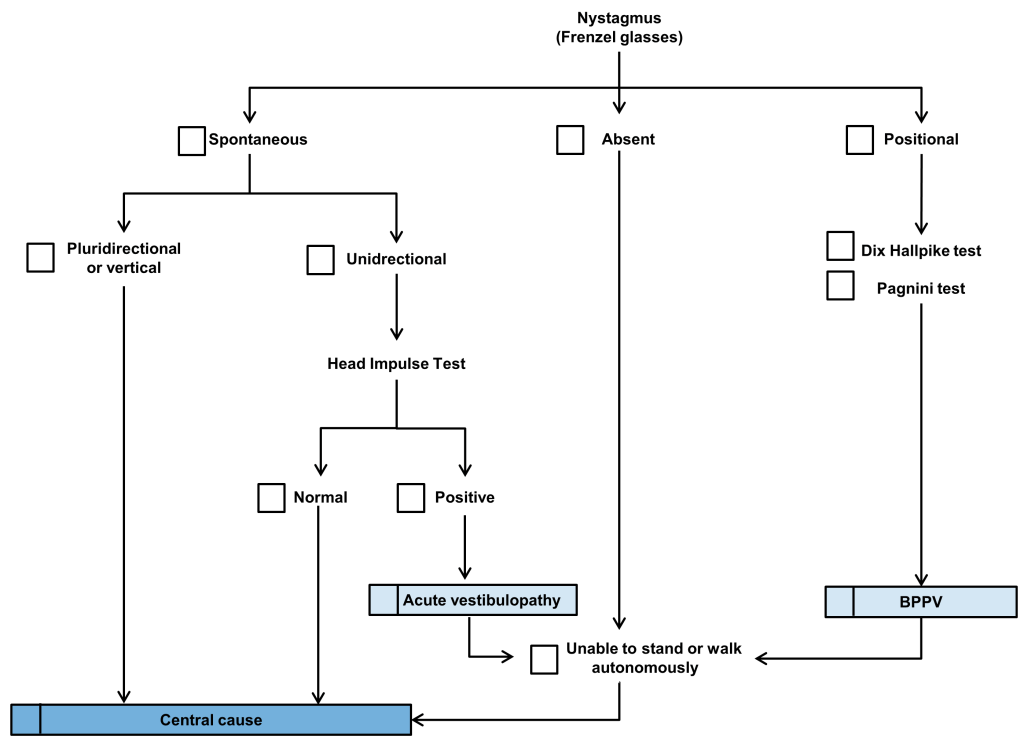
Standing Test
Hot off the press: Self-obtained vaginal swabs for sexually transmitted infection testing
- For the primary outcome, self-swabs had a sensitivity of 95% (95% CI= 88% to 99%) for the detection of NG/CT when com-pared to provider performed swabs. Secondary outcomes revealed an excellent kappa of 93%, and self-swab sensitivities for NG and CT were 97% and 94%, respectively
American Journal of Emergency Medicine
None
Annals of Emergency Medicine
The Emergency Medicine Physician Workforce: Projections for 2030
- 2% annual graduate medical education growth, 3% annual emergency physician attrition, 20% encounters seen by a nurse practitioner or physician assistant, and 11% increase in emergency department visits relative to 2018. This scenario would result in a surplus of 7,845 emergency physicians in 2030.
- Clinical protocol for ED patients with moderate to severe alcohol use disorder using oral naltrexone and extended-release intramuscular naltrexone together with substance use navigation. Identification of alcohol use disorder, a brief intervention, and initiation of naltrexone resulted in a 15% follow-up rate in formal addiction treatment. Future work should prospectively examine the effectiveness of naltrexone as well as the effect of substance use navigation for ED patients with alcohol use disorder.
- Low-threshold ED buprenorphine treatment implemented with a harm reduction approach and active navigation to outpatient addiction treatment was successful in achieving buprenorphine treatment for opioid use disorder in diverse California communities.
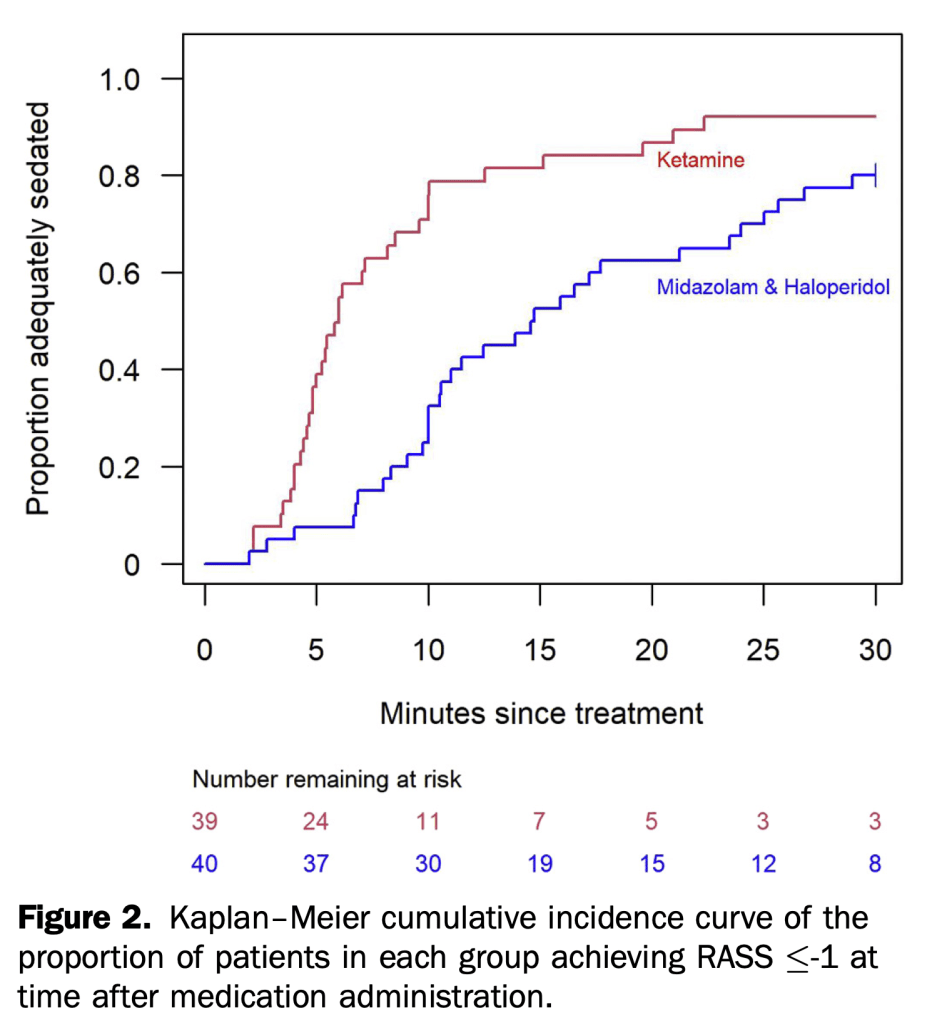
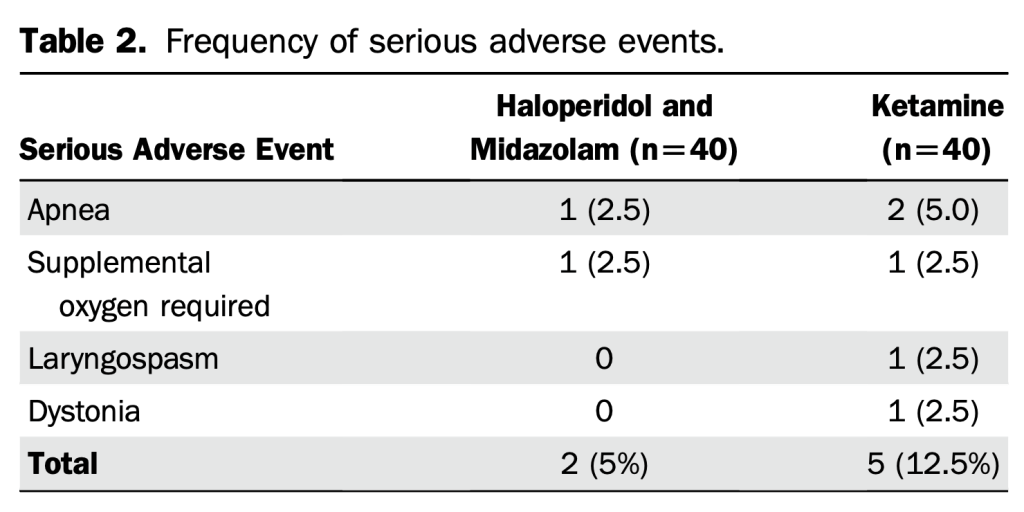
- In this randomized controlled trial of 80 adults, the median time to adequate sedation was significantly faster for ketamine 5mg/kg IM versus Midazolam 5mg IM/haloperidol 5mg IM (6 versus 15 minutes, respectively).
BMJ
Management of pneumonia in critically ill patients
Circulation
EMCRIT
None
Emergency Medicine Journal
None
EMRAP
- subxiphoid
- have someone count down from 10 seconds, remove probe and wipe with 2 to go
- >20% blasts, call oncology
JAMA
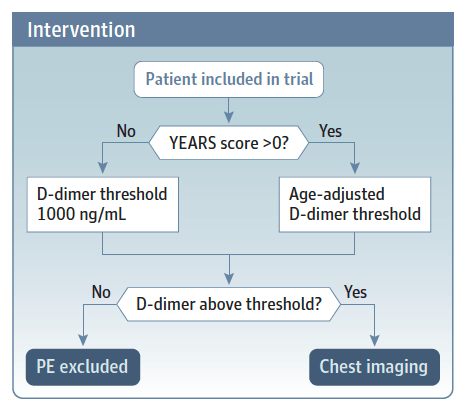
- Excluded:
- high probability of PE>50%
- low probability of PE with a PERC score of zero
- severe illness (resp distress, hypotension, o2 saturation <90%
- current antico-agulant treatment
- a current diagnosis of thromboembolism,
- pregnancy
Diagnostic Strategies for Pulmonary Embolism
- Intubation occurred in 34 (34.3%) randomized to high-flow oxygen therapy and in 51 (51.0%) randomized to conventional oxygen therapy (hazard ratio, 0.62; 95% CI, 0.39-0.96; P = .03). The median time to clinical recovery within 28 days was 11 (IQR, 9-14) days in patients randomized to high-flow oxygen therapy vs 14 (IQR, 11-19) days in those randomized to conventional oxygen therapy (hazard ratio, 1.39; 95% CI, 1.00-1.92; P = .047).
Association of Rivaroxaban vs Apixaban With Major Ischemic or Hemorrhagic Events in Patients With Atrial Fibrillation (no open access)
- Among Medicare beneficiaries 65 years or older with atrial fibrillation, treatment with rivaroxaban compared with apixaban was associated with a significantly increased risk of major ischemic or hemorrhagic events.
Contraception Selection, Effectiveness, and Adverse Effects
Journal of Emergency Medicine
None
Lancet
None
NEJM
Angiography after Out-of-Hospital Cardiac Arrest without ST-Segment Elevation
- No benefit
Pulmonary Arterial Hypertension
Spontaneous Intracranial Hypotension
PEDIATRICS
None
REBELEM
Meta-Analysis on Topical TXA for Epistaxis
- Janapala RN, et al. Efficacy of Topical Tranexamic Acid in Epistaxis: A Systematic Review and Meta-Analysis. Am J Emerg Med. Nov 2021.
- This meta-analysis highlights the importance of a head-to-head comparison of first line agents in the treatment of epistaxis. Knowing the efficacy of topical TXA compared to other first line vasoconstrictors from this study, it’s not an unreasonable approach to use it as a first line agent. The use of TXA in epistaxis should be left to the discretion of the emergency physician. Although, the NoPAC trial showed no difference in the use of topical TXA, that study was different in that direct pressure plus phenylephrine was used and only after failure were patients randomized to TXA vs placebo. Maybe a better strategy would be direct pressure PLUS TXA as a 1st line approach to epistaxis as it appears from this study that it does a better job in bleeding cessation when compared to other vasoconstrictors.
REBEL Core Cast 71.0 – Troubleshooting the Vent
- Dislodged- check ETT depth
- Obstruction- pass a suction catheter
- Pneumothorax- ultrasound linear probe
- Equipment failure- look for air leak, volume in more than volume returned
- Stacking of breaths/Dyssynchrony
Posterior Occlusion Myocardial Infarctions and STDmaxV1-4
- Not all occlusion myocardial infarctions (OMIs) present with classic ST-segment elevation (We have covered this on REBEL EM Before HERE, HERE, and HERE). OMIs of the “posterior” and “lateral” walls are the most commonly missed, with >50% of left circumflex occlusions (Posterior and lateral walls suppled by the circumflex artery)not receiving emergent reperfusion. These misses occur because isolated posterior OMIs do not result in classic ST-elevation ECG changes. Instead, posterior OMI results in ST depression which is maximal in V1 to V4 (alternatively, ST-depression of subendocardial ischemia is maximal in V5 to V6).
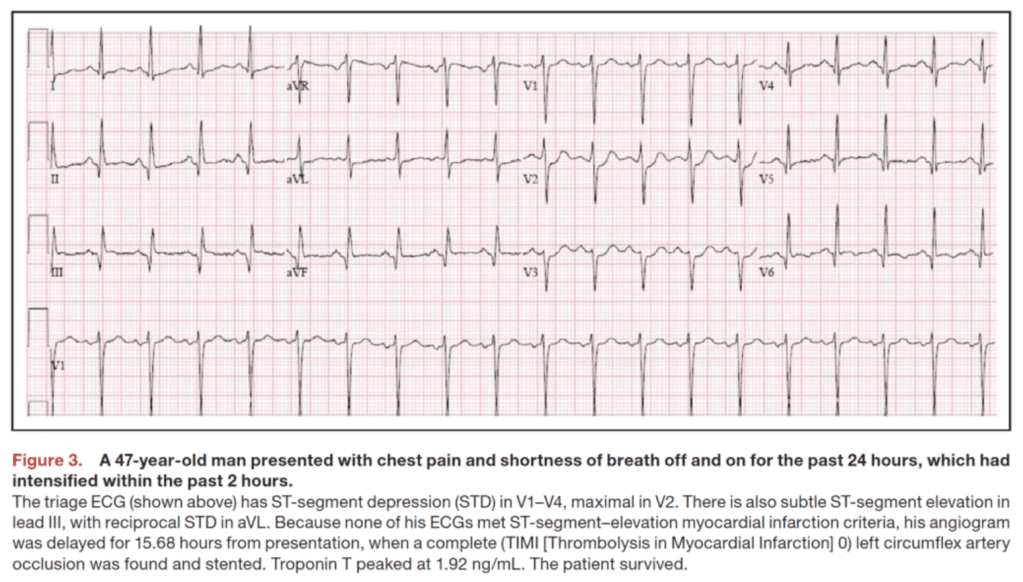
- In patients with symptoms suggestive of ACS in the ED, the specificity of STDmaxV1-4 was 97% for the diagnosis of posterior OMI and 96% for posterior OMI requiring PCI. This finding of STDmaxV1-4 is both highly accurate and sufficient without the need for routine posterior leads.