Contents
- Definition
- Epidemiology
- Pathogenesis
- Clinical Presentation
- Physical Exam
- Labs
- Differential Diagnosis
- Diagnosis
- Treatment
- Disposition
- References
_____________________________________________________________________________________________
Definition
_____________________________________________________________________________________________
- Giant cell arteritis (GCA) has replaced temporal arteritis (TA) as the preferred term due to the multiple vessels involved.
- Systemic inflammatory vasculitis of medium and large-sized arteries.
- Most feared complication is irreversible vision loss (8-20% of untreated GCA patients), which is nearly eliminated by prompt initiation of steroids.
_____________________________________________________________________________________________
Epidemiology
_____________________________________________________________________________________________
- Most common vasculitis affecting adults in western countries.
- Almost never seen below 50 yo (of 1,435 pooled GCA cases, there are only 2 documented cases of GCA in patients younger than 50 years.)
- Mean age of onset is 75 years.
- More common in females with a ratio of about 2 to 1.
- Incidence is highest in individuals of Scandinavian ancestry.
_____________________________________________________________________________________________
Pathogenesis
_____________________________________________________________________________________________
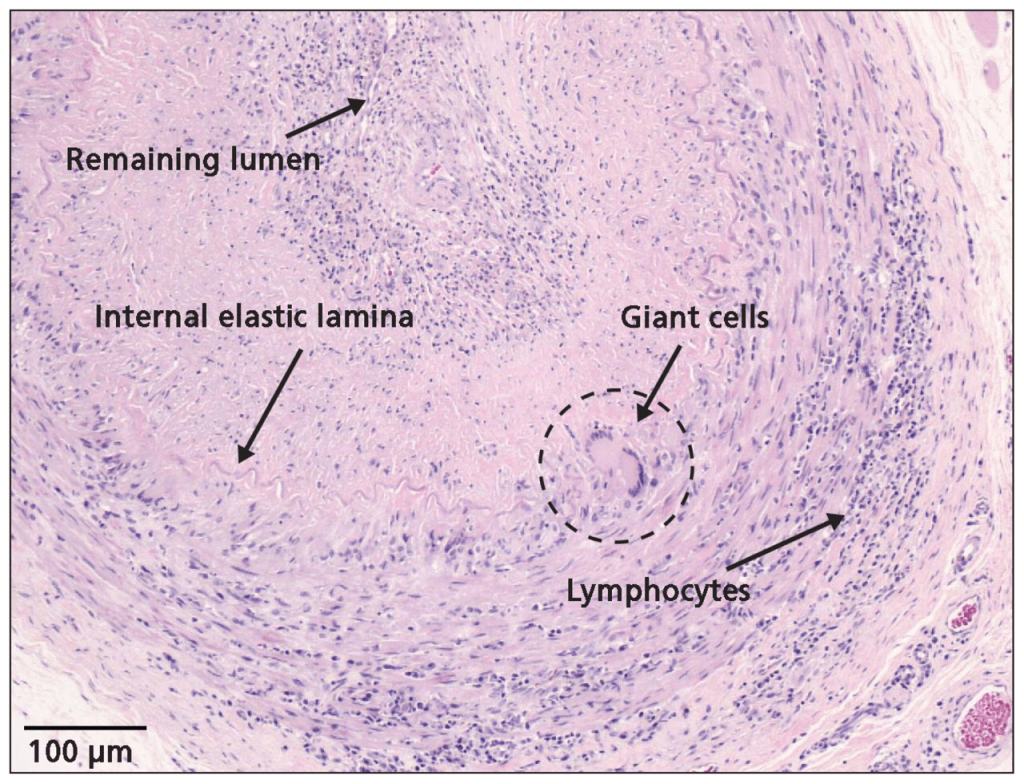
- Exact cause is unknown.
- Thought to be an abnormal immune response to endothelial injury.
- Granulomatous inflammation within the wall layers of medium and large arteries.
- Granulomatous infiltrates are composed of CD4 T cells and highly activated macrophages and multinucleated giant cells.
- Giant cells are a mass formed by the union of several distinct cells (usually histiocytes), often forming a granuloma (clump of macrophages).
- Cause of blindness is usually occlusion of the posterior ciliary artery, a branch of the ophthalmic artery from the internal carotid artery, and the main arterial supply to the optic nerve.
_____________________________________________________________________________________________
Clinical Presentation
_____________________________________________________________________________________________
Presentation is inconsistent (not always temporal headache)
- Onset-
- 2/3 of cases are gradual onset but 1/3 can occur over a few days
- Constitutional symptoms
- 50% have low-grade fever, 15% have fever >102
- Headache
- Seen in 2/3 of patients
- Classically temporal location but location not reliable
- More important than location is that it is a NEW headache and >50yo
- Ocular involvement (many possible presentations)
- Transient vision loss (amaurosis fugax) monocular or rarely binocular.
- Abrupt partial field defect or temporary curtain effect in the field of one eye
- Permanent vision loss
- May be partial or complete
- May be unilateral or bilateral
- Diplopia in 5% of GCA patients
- Transient vision loss (amaurosis fugax) monocular or rarely binocular.
- Jaw claudication
- Mandibular pain or fatigue brought on by chewing and relieved by stopping
- Trismus-like symptom, perceived or actual limitation of TMJ movement
- Nearly 50% of GCA patients experience jaw claudication
- Jaw claudication was the symptom most highly associated with a positive biopsy
Likelihood ratios for various signs and symptoms of TA
When to suspect giant cell arteritis (from UPTODATE)
- Patient> 50 yo with one of the following symptoms or signs:
- New headaches
- Abrupt onset of visual disturbances, especially transient/permanent monocular visual loss
- Jaw claudication
- High ESR and/or high CRP
- Temporal artery abnormalities such as tenderness to palpation, decreased pulse amplitude, presence of nodules
_____________________________________________________________________________________________
Physical Exam
_____________________________________________________________________________________________
Exam is usually normal but look for the following:
- Cardiovascular
- Abnormal pulses (carotid, brachial, radial, femoral, pedal) or discrepant blood (>10mm Hg systolic or diastolic) in the arms can occur with GCA.
- Temporal Artery
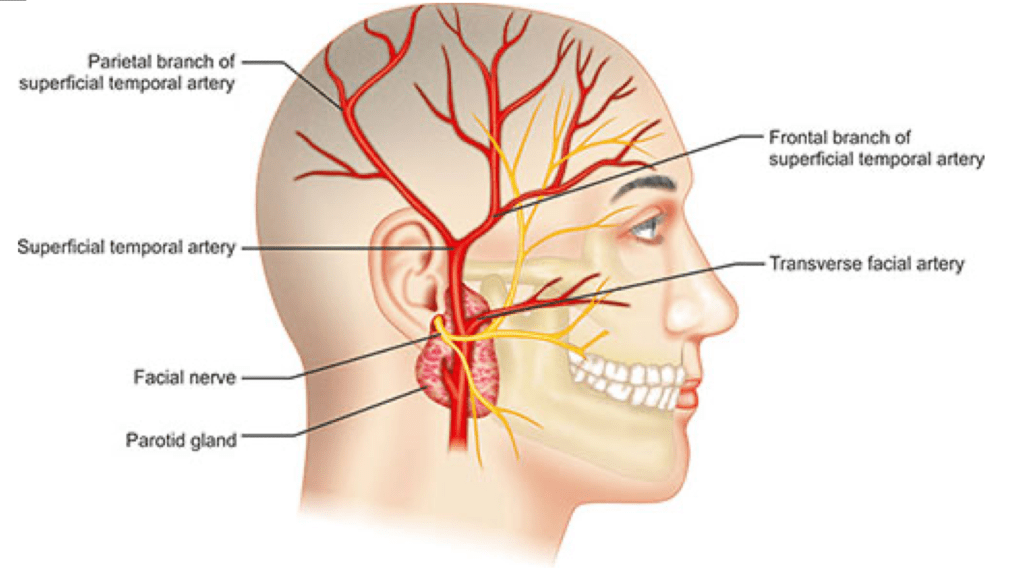
- The frontal or parietal branches of the superficial temporal arteries may be thickened, prominent (see picture below), nodular, tender, or occasionally erythematous. Pulses may be decreased or absent.
- Exam tips
- Palpate the scalp along the general course of the superficial, frontal and parietal branches (see diagram below).
- Document no scalp tenderness or prominent temporal arteries.
- Document normal temporal artery pulse (palpable anterior to the tragus).

- Ocular findings
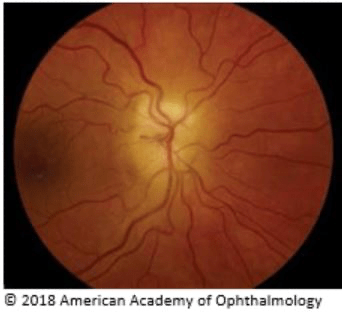
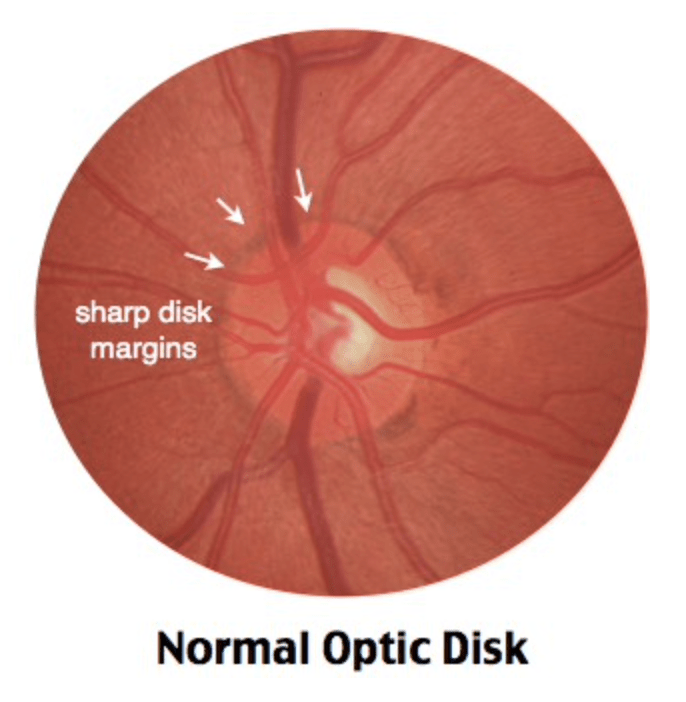
- Fundoscopic exam- swollen, pale disc with blurry margins (see picture below).
- Exam tips
- Document visual acuity
- Can use MDCalc Snellens chart held at 4ft.
- Perform fundoscopic exam if patient has visual complaints.
- Document visual acuity
- Musculoskeletal findings
- Patients with polymyalgia rheumatica (PMR), may have decreased range of motion of the shoulders, neck, and hips, especially in the morning.
- May have distal synovitis, especially wrists and mcp joints.
_____________________________________________________________________________________________
Labs
_____________________________________________________________________________________________
Get both ESR and CRP
- EMRAP recommends both- March 2019.
- UPTODATE recommends both- February 2022.
- 2012 Kermani study
- Normal ESR (<23 mm/hr in men and <30 in women)- 84% sensitive.
- Normal CRP (<8mg/L, 0.8mg/dL)- 86% sensitive.
- Normal ESR and CRP- 96% sensitive.
- Abnormal ESR OR CRP- 30% specific.
- Abnormal ESR AND CRP- 41% specific.
- Various normal ESR and CRP values proposed, no accepted number (use your hospital’s normal).
- Age adjusted ESR normal formula: Men- age/2, Women- (age+10)/2.
- Bottom line–
- Labs are nonspecific and will not rule in or out the diagnosis.
- Neither test is necessary to start steroids or to discharge patient, but results can help risk stratify the patient for whether or not to start steroids (see disposition section below).
- Many experts recommend getting them and physician you refer the patient to will appreciate if labs are performed when the patient is referred.
_____________________________________________________________________________________________
Differential Diagnosis
_____________________________________________________________________________________________
- Acute Angle-Closure Glaucoma
- Cervical Artery Dissection
- Herpes Zoster
- Iritis/Uveitis
- Migraine
- Non-Arteritic Ischemic Optic Neuropathy
- Optic Neuritis
- Postherpetic Neuralgia
- Retinal Artery Occlusion
- Retinal Vein Occlusion
- Sinusitis
- TIA/Stroke
_____________________________________________________________________________________________
Diagnosis
_____________________________________________________________________________________________
Temporal Artery Biopsy
- Gold standard
- Outpatient procedure
- Done by an ophthalmologist or vascular surgeon with local anesthesia.
- Typically start steroids and refer for biopsy to confirm diagnosis within 2-4 weeks unless acute vision loss.
Color Doppler Ultrasonography and MRI with contrast
- Alternative or complement to biopsy but only when performed by clinicians with extensive experience in this technique.
- 2016 JAMA review of 10 studies showed good specificity but lower and wider sensitivity.
- CDUS specificity 78%-100%
- MRI specificity 73%-97%
- Sensitivity varied from 55-100%.
- May use non-invasive imaging workup to rule in and if negative proceed to biopsy to rule out unless post test suspicion very low after non-invasive workup.
- Not typically done as an inpatient, refer to PCP/Rheum/Neuro/Referral hospital within 1 week to choose workup strategy and arrange within 2-4 weeks as long as no visual complaints.
_____________________________________________________________________________________________
Treatment
_____________________________________________________________________________________________
No vision loss
- Per UPTODATE (Feb 2022), if GCA is “strongly suspected” and there is no vision loss, treat with steroids.
- Prednisone 1mg/kg (max 60mg) PO QD
- Begin gradual taper after 2 wks, but often require steroids for 1 year
- May be safest to prescribe 5 day course and recommend follow-up with PCP or Neurology or Rheumatology or Ophthalmology or a Referral Hospital to defer decisions about whether a longer course is indicated.
Vision Loss
- Per UPTODATE (Feb 2022), if there is a “strong suspicion” that GCA is the cause of visual signs or symptoms, treat with IV steroids x 3 days followed by po prednisone.
- IV methylprednisolone (Solu-Medrol) 500-1000mg IV QD x 3 days
_____________________________________________________________________________________________
Disposition
_____________________________________________________________________________________________
GCA considered but both ESR and CRP negative and no vision loss
- If both ESR and CRP negative and pre-test suspicion for GCA was not high, no need to start steroids, simply refer patient to PCP for outpatient follow-up within 1 week, cautioning the patient that the diagnosis of GCA is still not ruled out because 4% of GCA will have negative ESR and CRP.
GCA considered but ESR and CRP equivocal and no vision loss
- If ESR and CRP have mixed results consider shared decision making with patient, discussing risk benefit of steroids
- Explain GCA diagnosis is outpatient (biopsy or CDUS or MRI), and current suspicion not high.
- 15-20% risk of eventual permanent vision loss if patient has GCA and gets no treatment.
- Treatment Risk- roughly doubled risk of sepsis, heart failure and GI bleed when steroids taken for 5-30 days (Annals of IM 2020).
- Benefit- no placebo controlled trials but based on retrospective studies, UPTODATE states steroids reduce risk of blindness to <1% if patient has GCA with intact vision at the time of steroid initiation.
- Recommend follow-up with PCP or Neurology or Rheumatology or Ophthalmology or a Referral hospital within 5 days.
GCA strongly suspected but no vision loss
- Start Prednisone
- Recommend follow-up with PCP or Neurology or Rheumatology or Ophthalmology or a Referral hospital within 5 days.
GCA strongly suspected, with transient or permanent vision loss
- If there is a strong suspicion of GCA as the cause of threatened (transient) or established vision loss
- IV steroids- methylprednisolone (Solu-medrol) 500-1000 IV QD x 3d
- Consult Neurology and admit if certain that the cause of vision loss is GCA
- If cause of vision loss in doubt consult ophthalmology
- Transfer for higher level of care if unable to get ophthalmology consult and cause of vision loss in doubt
_____________________________________________________________________________________________
References
_____________________________________________________________________________________________
Amber M et al. Temporal Arteritis, StatPearls, December 2021
Butterfield M. Can Giant Cell Arteritis Be Ruled Out in the ED? EMDOCS. Nov 2015
Buttgerit, F. Polymyalgia Rheumatica and Giant Cell Arteritis. A Systematic Review. JAMA 2016.
Claudius I. Giant Cell Arteritis. EMRAP. March 2019
Docken W. Treatment of giant cell arteritis. UPTODATE March 8 2022
Jhun P et al. Giant Cell Arteritis: Read the Fine Print! Annals of Emergency Medicine. May 2015.
Salvarani C. Clinical manifestations of giant cell arteritis. UPTODATE. Feb 2022.
Salvarani C. Diagnosis of Giant Cell Arteritis. UPTODATE Feb 2022.